Source from Kelvin A. Power’s Facebook on August 3, 2019
အရင်အပိုင်း(၁)မှာတုံးကကျွန်တော်က(Type-2 Diabetes)ဟာအသဲရောဂါ(Liver Disease) ပါလို့တစ်ခြားလူတွေတခါမှမပြောဖူးတဲ့ထူးဆန်းတဲ့စကားကိုပြောလိုက်တော့၊ဒီခေတ်ခပ်ညံ့ညံ့အရင်းရှင်ဆေးပညာမှာလမ်းဆုံးနေကြတဲ့ပုဂ္ဂိုလ်တွေလက်မခံချင်ကြဘူး။ကျွန်တော်ဘယ်လိုသိလဲဆိုတော့ကျွန်တော့်(Friend)တစ်ယောက်ကအပိုင်း(၁)ပို့စ်ကို(ဆီးချိုဝေဒနာသည်များအတွေ့အကြုံဖလှယ်ရာGroup)မှာသွားပြီးတင်တော့(admin)ကဖြုတ်ချပြစ်လိုက်တယ်လို့ပြန်ပြောပြတယ်။ကျွန်တော်စိတ်မကောင်းဖြစ်မိတာကအဲဒီလိုဉာဏ်မမှီအသိဉာဏ်နည်းတဲ့ခပ်တုံးတုံး(admin)တယောက်အတွက်နဲ့အဲဒီ(group)မှာရှိနေတဲ့ဆီးချိုဝေဒနာသည်တွေအတွက်အသက်လောက်အရေးကြီးတဲ့အသိထူးဗဟုသုတတွေမသိလိုက်မဖတ်လိုက်ရတာကိုပဲသနားနေမိတာပါ။သာမာန်အသိပညာအတတ်ပညာလောက်ကတော့လူတိုင်းနားလည်လွယ်ပါတယ်။ဒါပေမဲ့ထူးခြားနေတဲ့အသိထူးတခုကြတော့သာမန်လောက်သိတဲ့လူတွေကသူတို့ဉာဏ်နဲ့မမှီတော့လက်မခံချင်ကြတော့ဘူး။တကယ်တော့လောကမှာသိခဲမှသာပညာခေါ်တာပါ။သူများသိသလောက်ပဲသိနေရင်ပညာမခေါ်သလိုဘာမှလဲအသုံးမဝင်လှပါဘူး။သူများထက်ထူးပြီးသိမှသာတန်ဖိုးရှိပြီးလူ့အကျိုးပြုနိုင်တာပါ။(Type-2 Diabetes)ဟာအသဲရောဂါ(Liver Disease)ဆိုတာကိုသိရင်ဒီရောဂါကိုအမြစ်ပြတ်အောင်ကုရတာလွယ်လွယ်လေးပါ။အနာသိရင်ဆေးရှိပါတယ်။အနာမသိရင်ဒါမှမဟုတ်တလွဲသိနေရင်သာဒုက္ခရောက်ကြရတာပါ။
————–
(Type-2 Diabetes)ဟာအသဲရောဂါ(Liver Disease) ဆိုတာကိုလက်မခံတဲ့လူတွေရှိရင်ကျွန်တော်မေးတာလေးကိုဖြေကြည့်စေချင်ပါတယ်။ကျွန်တော်တို့ဘာကြောင့်ဆီးချိုဖြစ်ရတာလဲ?။အဲဒီလိုမေးရင်လူတွေကဘယ်လိုဖြေမလဲဆိုတော့(Glucose, Carbohydrate)ပါတဲ့အချိုတွေသိပ်စားလို့ဖြစ်တယ်လို့ပြန်ဖြေကြလိမ့်မယ်။ဒီလိုကတော့(၅)နှစ်ကလေးတွေတောင်ဖြေတတ်ပါတယ်။အဲဒါဆိုရင်ထပ်မေးချင်တာကအချိုမကြိုက်တဲ့၊မစားတဲ့လူဆိုရင်ကောဆီးချိုမဖြစ်နိုင်တော့ဘူးလား?အချိုကြိုက်တဲ့လူတိုင်းရောဆီးချိုဖြစ်သလား?လို့ထပ်မေးရင်ဘယ်လိုဖြေမလဲ?ရှင်းရှင်းပြောရရင်ဆီးချိုရောဂါရတယ်ဆိုတာကအချို(Glucose) စားတာမစားတာနဲ့လဲမဆိုင်ဘူး။ကစီဓါတ်(Carbohydrate)စားတာမစားတာနဲ့လဲမဆိုင်ဘူး။အဆီ(fat)စားတာမစားတာနဲ့လဲမဆိုင်ဘူး။အချိုမစားလဲဆီးချိုဖြစ်ချင်ဖြစ်မယ်အချိုတွေကြိုက်သလောက်စားလဲဆီးချိုမဖြစ်ချင်ရင်မဖြစ်ဘူး။အဲဒါတွေအားလုံးကအသဲနဲ့ပဲဆိုင်တယ်။အသဲကအဆိပ်သင့်နေရင်ဘာစားစားမစားစားဆီးချိုဖြစ်မယ်။အသဲကိုသာကောင်းအောင်၊ကျန်းမာအောင်ထားနိုင်ရင်ဘာစားစား(Type-2 Diabetes)ဖြစ်မလာနိုင်ပါဘူး။ဒီလောက်ဆိုရှင်းပါတယ်နော်။
——————
ကမ္ဘာပေါ်မှာလူသားရယ်လို့ဖြစ်တည်လာခဲ့တာကမ္ဘာဦးကျောက်ခေတ်ကတည်းကနှစ်ပေါင်းသန်းနဲ့ချီရှိနေပါပြီ။(Type-2 Diabetes)ဆီးချိုရောဂါစဖြစ်တယ်ဆိုတာကနှစ်(၂၀၀)တောင်မပြည့်သေးပါဘူး။ဟိုးအရင်တုံးနှစ်ပေါင်းများစွာတုံးကကဘာလို့ဒီရောဂါမဖြစ်ပဲအခုမှဘာလို့ထဖြစ်ရတာလဲ?။ကျွန်တော်တို့ခန္ဓာကိုယ်ထဲမှာဒီရောဂါမဖြစ်အောင်ကာကွယ်ပေးဖို့သဘာဝကပေးထားတဲ့ကာကွယ်ရေးစနစ်တခုခုပါမလာဘူးလား?။ဒီရောဂါဖြစ်လာတာဟာဘယ်သူ့မှာတာဝန်ရှိသလဲ?ဘယ်စနစ်ချွတ်ယွင်းသွားလို့လဲလို့မေးရင်ဒီခေတ်ဆေးပညာရှင်တွေဘယ်လိုဖြေကြမလဲ?။အဖြေကတော့ကျွန်တော်တို့ခန္ဓာကိုယ်ထဲမှာဆီးချိုရောဂါမဖြစ်အောင်မိခင်သဘာဝကပေးထားတဲ့အင်္ဂါအစိတ်အပိုင်းနဲ့ကာကွယ်ရေးစနစ်တွေပါကိုပါလာပါတယ်။အဲဒါကိုကျွန်တော်တို့တွေမသိလို့နားမလည်လို့၊အဲဒီစနစ်ကြီးမပျက်စီးသွားအောင်မထိန်းသိမ်းတတ်ကြလို့သာဒုက္ခဖြစ်ကြရတာပါ။အဲဒါကတော့တစ်ခြားမဟုတ်ပါဘူး(Liver)လို့ခေါ်တဲ့အသဲပါပဲ။အသဲကောင်းနေရင်၊ကျန်းမာနေရင်အချိုမကလို့ဘာကြီးပဲစားစားဆီးချိုရောဂါဆိုတာမဖြစ်ပါဘူး။မိခင်သဘာဝကဒီရောဂါကိုကာကွယ်ဖို့လုပ်ငန်းဆောင်တာတွေအသဲထဲမှာထည့်ထားပေးပြီးသားပါ။ဒီအသဲကကောင်းကောင်းအလုပ်မလုပ်နိုင်တော့လို့၊သူပျက်စီးချွတ်ယွင်းနေလို့ဆီးချိုရောဂါဆိုတာဖြစ်လာရတာပါ။သူ့ကိုကျန်းမာသွားအောင်၊ပုံမှန်အလုပ်လုပ်နိုင်အောင်ပြုပြင်ကုသပေးလိုက်ရင်ဆီးချိုရောဂါဆိုတာမရှိတော့ပါဘူး။(Type-2 Diabetes)ဟာအသဲရောဂါ(Liver Disease)ပါလို့ပြောတာကိုလက်မခံချင်တဲ့လူတွေနောက်ပိုင်းမှာငြင်းမရတော့လိုလက်ခံလာရမှာပါ။အမှန်တရားဆိုတာလက်မခံလို့ကိုမရပါဘူး။
———————-
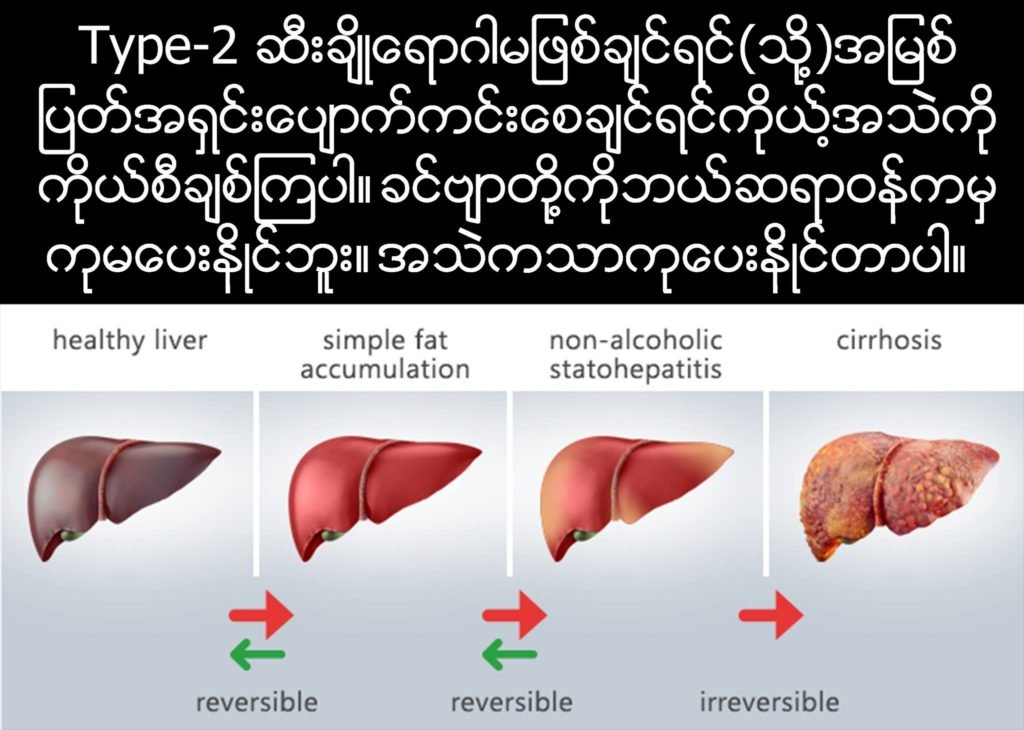
ကမ္ဘာပေါ်မှာ(Type-2 Diabetes)ရောဂါသည်တွေအားလုံးနီးပါးမှာအရက်မသောက်ပဲအသဲကိုအဆီဖုံးနေတဲ့ရောဂါ(Non Alcoholic Fatty Liver Disease, NAFLD)ရှိနေကြတယ်ဆိုတာ၊သုသေသနတွေတော်တော်များများကပြောနေကြပါပြီ။ဆီးချိုရောဂါသည်တွေအားလုံးပိန်ပိန်ဝဝ၊အသဲမှာအဆီကတော့အနဲနဲ့အများသာကွာတာပါလူတိုင်းရှိနေတတ်ကြပါတယ်။အဲဒီပြဿနာကစပြီးရောဂါတွေအမျိုးမျိုးဖြစ်ပေါ်လာရတာပါ။အသဲအဆီဖုံးတယ်ဆိုတာသာမညပြဿနာအသေးလေးမဟုတ်ပါဘူး။ဒါကို(Metabolic syndrome)လို့ခေါ်ပါတယ်။(Metabolic syndrome) ကြောင့်ဆီးချိုလောက်နဲ့ရပ်မသွားပဲအဆိုးဆုံးရောဂါဆိုးတွေအမျိုးမျိုးအဖုံဖုံမရေမတွက်နိုင်အောင်ဖြစ်လာနိုင်ပါတယ်။
———————————–
ပုံမှန်အားဖြင့်အသဲရဲ့လုပ်ဆောင်မှု့တွေအများကြီးထဲကအဓိကကျလှတဲ့လုပ်ဆောင်မှုစနစ်(၂)ခုအကြောင်းကိုအရင်ပြောပြချင်ပါတယ်။အဲဒါတွေကတော့သိုလောင်ထားတာတွေကိုလိုအပ်တဲ့အချိန်မှာပြန်လည်ဖြိုချထုတ်ယူအသုံးပြုနိုင်တဲ့ဖြိုချသုံးစွဲမှု့စနစ်(Catabolic)နဲ့ပိုနေတာတွေကိုပြန်ပြီးသိုလှောင်သိမ်းဆည်းရတဲ့သိုလှောင်သိမ်းဆည်းှမှုစနစ်(Anabolic)ပါ။သူတို့နှစ်ခုဟာတစ်ခုနဲ့တစ်ခုတိုက်ရိုက်ကြီးဆန့်ကျင်နေတဲ့သဘောသဘာဝတွေဖြစ်နေလို့ဘယ်တော့မှနှစ်ခုတပြိုင်တည်းမဖြစ်နိုင်သလိုအချိန်တိုင်းမှာလဲတခုမဟုတ်တခုကတော့ဖြစ်နေရပါတယ်။ဘယ်အချိန်မှာဘယ်သဘောဖြစ်နေရမလဲလို့ထိန်းချုပ်ခိုင်းစေနေတဲ့ဟော်မုန်းဓါတ်တွေကတော့အဓိကအားဖြင့်နစ်မျိုးရှိပါတယ်။အင်ဆူလင်(Insulin=I)နဲ့ဂလူဂိုဂွန်(glucagon=G) ဟော်မုန်းတွေပါ။ဒီနေရာမှာ၊အင်ဆူလင်(I)ဟော်မုန်းကသာဂလူဂိုဂွန်(G)ဟော်မုန်းကိုပြန်ပြီးထိန်းချုပ်ထားနိုင်တဲ့အတွက်၊အင်ဆူလင်(I)ဟော်မုန်းကသာပိုပြီးအဓိကကျနေလို့သူ့ကိုပဲအဓိကထားပြီးဆွေးနွေးသွားပါမယ်။
———————————-
လူတစ်ယောက်ဟာမနက်အိပ်ရာကထထခြင်းညကအိပ်ပျော်နေတဲ့အချိန်မှာအစားစားနေတာမဟုတ်လို့အစာမစားထားတဲ့အချိန်မှာအားအင်မပြတ်သွားအောင်အသဲကသကြားဓါတ်တွေကိုထုတ်ပေးထားနေရပါတယ်။၊ဖြိုချသုံးစွဲမှု့စနစ်(Catabolic)ဆိုတာအစာစားထားခဲ့တုံးကအသဲကစွမ်းအင်အဖြစ်သိုလောင်ထားတဲ့(liver glycogen)ကနေအစာမစားထားတဲ့အချိန်မှာစွမ်းအင်မပြတ်သွားရအောင်သကြားဓါတ်ထုတ်လုပ်ပေးသလိုခန္ဓာကိုယ်မှာရှိနေတဲ့အဆီ(adipose tissue)တွေကနေလဲအဆီတွေကိုဖျော်ချပြစ်ပြီးသုံးစွဲလို့ရမယ့်စွမ်းအင်စနစ်(Fat Catabolism)ကိုပြုလုပ်ပေးနေပါတယ်။
—————————-
ပုံမှန်အားဖြင့်လူတစ်ယောက်ဟာမနက်မိုးလင်းလာလို့အိပ်ရာကထပြီးဗိုက်ထဲမှာအစာမရှိသေးတဲ့(fasting)အချိန်မှာတစ်နေ့တာအတွက်ပထမဦးဆုံးသောနံနက်စာကိုကစီဓါတ်(Carbohydrate)ပါဝင်မှုများတဲ့အစားအသောက်တခုခုကိုစားလိုက်တယ်ဆိုကြပါစို့၊ကစီဓါတ်(Carbohydrate) များတဲ့အစားအသောက်တစ်ခုစားလိုက်တာနဲ့သွေးထဲမှာသကြားဓါတ်(Glucose)တက်လာပြီးခန္ဓာကိုယ်ကသကြားဓါတ်ကြောင့်အန္တရာယ်ဖြစ်တော့မယ်ဆိုတာကိုကြိုသိတော့သွေးထဲမှာသကြားဓါတ်(Glucose)ကိုပုံမှန်ထက်ပိုပြီးမရှိနေစေဖို့ပိုလျံနေတဲ့သကြားဓါတ်တွေကိုသွေးထဲကနေဖယ်ရှားပြစ်နိုင်ဖို့(Insulin)လို့ခေါ်တဲ့(Hormone)ဓါတ်ကို၊(Pancreases)ကနေထုတ်လုပ်ပေးရပါတယ်။(Insulin)လို့ခေါ်တဲ့ဟော်မုန်းဓါတ်ကခန္ဒာကိုယ်အစိတ်အပိုင်းအမျိုးမျိုးကိုရောက်ရှိသွားပြီးအင်္ဂါအစိတ်အပိုင်းအားလုံးကိုသွေးထဲကသကြားဓါတ်တွေကိုအမြန်ဆုံးစုပ်ယူအသုံးပြုဖို့တွန်းအားပေးလှုပ်ဆော်လိုက်သလိုတဖက်ကလဲအသဲဆီကိုရောက်ရှိသွားပါတယ်။အသဲဆီကိုအင်ဆူလင်ဟော်မုန်းရောက်သွားတာနဲ့ချက်ချင်းပဲအင်ဆူလင်ရဲ့ခိုင်းစေမှုကြောင့်အသဲရဲ့မနေ့ညကတည်းကတညလုံးလုပ်နေခဲ့တဲ့ဖြိုချသုံးစွဲမှု့စနစ်(Catabolic)စနစ်ကိုချက်ချင်းရပ်ပြစ်လိုက်ရပြီးတော့သကြားဓါတ်ကိုပြန်လည်သိမ်းဆည်းသိုလောင်တဲ့(Anabolic)စနစ်သို့ပြောင်းပြန်ပြောင်းလဲပြစ်ရပါတယ်။ဆိုလိုတာကအသဲရဲ့သကြားဓါတ်ထုတ်လုပ်မှုစနစ်(gluconeogenesis)ဆိုတဲ့ပုံမှန်လုပ်ငန်းစဉ်တွေကိုချက်ခြင်းရပ်လိုက်ပြီးတော့သကြားဓါတ်ကိုပြန်လည်သိမ်းဆည်းသိုလှောင်မှုစနစ်(Anabolic)ကိုချက်ခြင်းပြောင်းပြစ်လိုက်ရတော့တာပဲ။
———————
အသဲမှာသိမ်းဆည်းသိုလှောင်မှု့စနစ်(Anabolic)အသက်ဝင်လာတော့ဆီးချိုမဖြစ်ရအောင်သွေးထဲမှာရှိနေတဲ့(Glucose)သကြားဓါတ်တွေကိုအသဲရဲ့(Liver Glycogen)အဖြစ်သိမ်းဆည်းမှု(Glycogenesis)နှင့်အတူထိုသကြားဓါတ်ကိုအဆီအဖြစ်ပြောင်းလဲပြစ်ပြီးခန္ဓာကိုယ်တွင်းအဆီအဖြစ်သိမ်းဆည်းသိုလှောင်မှုစနစ်(Fat Anabolism)ကိုချက်ခြင်းပြောင်းလဲသွားရတာပါပဲ။အသဲကသွေးထဲမှာဝင်လာတဲ့သကြားဓါတ်အားလုံးကိုအဆီတွေအဖြစ်ပြောင်းလဲဖို့(lipogenesis)လုပ်တယ်။အဲဒီအဆီတွေကိုခန္ဒာကိုယ်အနှံ့အပြားမှာသိုလောင်သိမ်းဆည်းထားနိုင်ဖို့ခန္ဓာကိုယ်အနှံ့အပြားသို့သယ်ယူပို့ဆောင်ပေးဖို့(Taxi)နဲ့တူတဲ့သယ်ဆောင်ပေးမဲ့ပရိုတိန်းဖြစ်တဲ့(VLDL)လို့ခေါ်တဲ့ကော်လက်စထရော(Cholesterol)တွေကိုပါအသဲကတခါတည်းထုတ်လုပ်ပေးတော့တယ်။ပုံမှန်အားဖြင့်ဒီ(VLDL)ကော်လက်စထရောတွေကအသဲဆီကအဆီတွေကိုခန္ဒာကိုယ်အနှံ့အပြားအစိတ်အပိုင်းအသီးသီးကိုသယ်ဆောင်သွားပြီးသိုလှောင်သိမ်းဆည်းထားလိုက်ကြတယ်။
———————————-
ဒီစနစ်ဟာကမ္ဘာဦးကတည်းကရှိလာခဲ့တဲ့စနစ်ဟောင်းပါ၊အသစ်မဟုတ်ပါဘူး။အစားအသောက်မှာသကြားဓါတ်များတိုင်းသွေးထဲမှာ(Glucose)တက်လာမယ်။သွေးထဲမှာဂလူးကို့စ်တက်လာတိုင်းအင်ဆူလင်ဟော်မုန်းရဲ့ခိုင်းစေမှုကြောင့်အသဲကအဲဒီကလူးကို့စ်ကိုအဆီအဖြစ်ပြောင်းလဲပြီး၊(VLDL)ကော်လက်စထရောတွေရဲ့အကူအညီနဲ့အသဲထဲကထုတ်ယူသယ်ဆောင်သွားပြီး၊ခန္ဒာကိုယ်အနှံ့အပြားမှာအဆီတစ်ရှုးတွေအဖြစ်သိုလှောင်ထားမယ်။ဒီလိုသိုလှောင်လိုက်ရင်သွေးထဲကသကြားဓါတ်အမြဲပြန်လျှော့သွားသလိုတဖက်ကလဲခန္ဓာကိုယ်အစိတ်အပိုင်းတွေမှာအဆီတက်လာမယ်။ဆိုလိုတာကအသဲကသာပုံမှန်အလုပ်လုပ်ပေးနေနိုင်ရင်သကြားဓါတ်တွေများများစားတိုင်းအဆီတွေတက်တက်ပြီးတဖြေးဖြေးပိုပြီးဝဝလာမယ်။ဝိတ်တွေအများကြီးတက်တက်လာမယ်။သွေးထဲမှာတော့ဂလူးကိုစ့်ကတော့ပုံမှန်ပဲရှိနေမယ်။အသဲကသာပုံမှန်အလုပ်ကောင်းကောင်းလုပ်နေရင်ဆီးချိုဘယ်လိုဖြစ်နိဲင်မလဲ။?ဝတာတော့ဝလာမယ်။ဆီးချိုတော့ဖြစ်လာစရာအကြောင်းမရှိပါဘူး။ရှင်းအောင်ပြောရရင်ကစီဓါတ်ခေါ်သကြားဓါတ်(Carbohydrate)အလွန်စားတဲ့လူဟာအသဲပေါ်မှုတည်ပြီးဆိုးကျိုးသုံးမျိုးဖြစ်လာနိုင်ပါတယ်။ဆီးချိုမဖြစ်ပဲနဲ့ကိုယ်အလေးချိန်တက်ပြီးဝချင်ဝလာမယ်။ဒါမှမဟုတ်မဝပဲနဲ့လဲဆီးချိုဖြစ်ချင်ဖြစ်လာမယ်။ဒါမှမဟုတ်ဝလဲဝဆီးချိုလဲဖြစ်ချင်ဖြစ်မယ်။အဲဒါတွေအားလုံးဘာဖြစ်ရမလဲဆိုတာကတော့မိမိရဲ့အသဲအပေါ်မှာပဲအဓိကကျမူတည်နေတာပါ။တခုမှတော့မကောင်းပါဘူး။ဝလာတာလဲမကောင်းဘူး။ဆီးချိုလဲမကောင်းဘူး။ကစီဓါတ်ခေါ်သကြားဓါတ်(Carbohydrate)ကိုအလွန်အကျွံမစားတာကတော့အကောင်းဆုံးပါပဲ။ဒါပေမဲ့ဒီနေရာမှာဆိုလိုချင်တာကကစီဓါတ်ခေါ်သကြားဓါတ်ကိုများများစားဖို့မစားဖို့ကိုပြောချင်နေတာမဟုတ်ဘူး။အသဲကောင်းနေရင်ကစီဓါတ်ခေါ်သကြားဓါတ်များများစားလဲဆီးချိုမဖြစ်ဘူးဝပဲဝလာမယ်လို့အဓိကပြောချင်တာပါ။
——–
ထပ်ရှင်းအောင်ပြောရရင် ကစီဓါတ်ခေါ်သကြားဓါတ်(Carbohydrate)ကြောင့်ဆီးချိုလုံးဝမဖြစ်ဘူးလို့ကျွန်တေ်မဆိုလိုဘူး။ကျွန်တော်ဆိုလိုချင်တာကကစီဓါတ်ခေါ်သကြားဓါတ်(Carbohydrate)ဟာဆီးချိုဖြစ်စေနိုင်တဲ့အကြောင်းအရင်းတွေထဲကတခုအပါအဝင်ဆိုတာတော့မှန်ပါတယ်ဒါပေမဲ့ဒီအကြောင်းတခုတည်းကြောင့်ဆီးချိုဖြစ်တာတော့မဟုတ်သေးဘူး။တခြားအကြောင်းတွေလဲညီညွတ်မှဖြစ်တယ်။မျိုးစေ့တစ်စေ့ကိုချစိုက်လိုက်လို့သစ်ပင်တပင်ပေါက်လာရင်၊မျိုးစေ့ကြောင့်အပင်ပေါက်ပါတယ်လို့ပြောရင်မှားတော့မမှားပါဘူး။ဒါပေမဲ့မျိုးစေ့ချစိုက်လိုက်တိုင်းတော့အပင်မပေါက်ပါဘူး။မျိုးစေ့တစ်စေ့အပင်ပေါက်ဖို့ရာ၊မြေ၊ရေ၊အပူချိန်၊စိုထိုင်းမှု၊သြဇာဓါတ်စသည့်တခြားအကြောင်းတရားတွေလဲညီညွတ်ဖို့လိုအပ်ပါသေးတယ်။
———————-
ဒီနေရာမှာကစီဓါတ်ခေါ်သကြားဓါတ်(Carbohydrate)ကြောင့်ဆီးချိုဖြစ်တယ်ဆိုတာမှန်တော့မှန်တယ်။ဒါပေမဲ့အသဲကောင်းနေရင်၊အသဲကျန်းမာနေရင်မဖြစ်ပါဘူး။ဒါကြောင့်အရေးတကြီးသိဖို့လိုအပ်တာကအသဲဘာလို့မကောင်းတာလဲ၊ဘာလို့ပျက်စီးသွားတာလဲ၊ဘာလို့ပုံမှန်အလုပ်မလုပ်တာလဲ။အသဲပြန်ကောင်းလာအောင်၊အသဲကျန်းမာလာအောင်၊ပုံမှန်အလုပ်လုပ်လာအောင်ဘာတွေလုပ်ရမလဲ။အဲဒီလိုလုပ်ပေးလိုက်ရင်ကော(Type2, Diabetes)ကနေအရှင်းပျောက်ပြီးပြန်ကောင်းလာနိုင်မလား?ဆိုတဲ့မေးခွန်းတွေဟာအလွန်စိတ်ဝင်စားစရာကောင်းပြီးတန်ဖိုးသိပ်ကြီးတဲ့မေးခွန်းတွေဖြစ်နေပါတယ်။ကြိုတင်ပြီးပြောချင်တာလေးတခုကတော့ဒီနည်းနဲ့ဆိုရင်နှစ်ပေါင်း(၄၀)လောက်(Type2, Diabetes)ဖြစ်ပြီးပြန်ကောင်းလာတဲ့လူတွေတောင်ရှိနေပါတယ်။နောက်ပို့စ်တွေမှာတိတိကျကျလေးအဖြေပေးပါမယ်။အခုတော့နားပါဦးမည်။
Kelvin Albert Power
(Nutrition Specialist, Florida, USA)
PS==>
အခုရေးထားတာကအပိုင်း(၂)ပါ။အရင်ရေးထားတဲ့အပိုင်း(၁)ကိုလဲပြန်ပြီးရှာဖတ်စေချင်ပါတယ်။အပိုင်း(၁)Links ကိုဒီမှာယူပါ
https://www.facebook.com/kelvin.power.1675/posts/124887625454320
—————-
1. Petäjä EM, Yki-Järvinen H. Definitions of Normal Liver Fat and the Association of Insulin Sensitivity with Acquired and Genetic NAFLD-A Systematic Review. Int J Mol Sci. 2016:17. [PMC free article] [PubMed] [Google Scholar]
2. Lonardo A, Lombardini S, Scaglioni F, Carulli L, Ricchi M, Ganazzi D, Adinolfi LE, Ruggiero G, Carulli N, Loria P. Hepatic steatosis and insulin resistance: does etiology make a difference? J Hepatol. 2006;44:190–196. [PubMed] [Google Scholar]
3. Ballestri S, Nascimbeni F, Romagnoli D, Lonardo A. The independent predictors of non-alcoholic steatohepatitis and its individual histological features.: Insulin resistance, serum uric acid, metabolic syndrome, alanine aminotransferase and serum total cholesterol are a clue to pathogenesis and candidate targets for treatment. Hepatol Res. 2016;46:1074–1087. [PubMed] [Google Scholar]
4. Ballestri S, Zona S, Targher G, Romagnoli D, Baldelli E, Nascimbeni F, Roverato A, Guaraldi G, Lonardo A. Nonalcoholic fatty liver disease is associated with an almost twofold increased risk of incident type 2 diabetes and metabolic syndrome. Evidence from a systematic review and meta-analysis. J Gastroenterol Hepatol. 2016;31:936–944. [PubMed] [Google Scholar]
5. Adinolfi LE, Rinaldi L, Guerrera B, Restivo L, Marrone A, Giordano M, Zampino R. NAFLD and NASH in HCV Infection: Prevalence and Significance in Hepatic and Extrahepatic Manifestations. Int J Mol Sci. 2016;17 [PMC free article] [PubMed] [Google Scholar]
6. Guaraldi G, Stentarelli C, Orlando G, Zona S, Carli F, Ballestri S, Lonardo A, Squillace N, Loria P. Nonalcoholic fatty liver disease in HIV-infected persons: epidemiology and the role of nucleoside reverse transcriptase inhibitors. J Acquir Immune Defic Syndr. 2010;53:278; author reply 278–281. [PubMed] [Google Scholar]
7. Guaraldi G, Lonardo A, Ballestri S, Zona S, Stentarelli C, Orlando G, Carli F, Carulli L, Roverato A, Loria P. Human immunodeficiency virus is the major determinant of steatosis and hepatitis C virus of insulin resistance in virus-associated fatty liver disease. Arch Med Res. 2011;42:690–697. [PubMed] [Google Scholar]
8. Younossi ZM, Koenig AB, Abdelatif D, Fazel Y, Henry L, Wymer M. Global epidemiology of nonalcoholic fatty liver disease-Meta-analytic assessment of prevalence, incidence, and outcomes. Hepatology. 2016;64:73–84. [PubMed] [Google Scholar]
9. Bertolotti M, Lonardo A, Mussi C, Baldelli E, Pellegrini E, Ballestri S, Romagnoli D, Loria P. Nonalcoholic fatty liver disease and aging: epidemiology to management. World J Gastroenterol. 2014;20:14185–14204. [PMC free article] [PubMed] [Google Scholar]
10. Bruno S, Maisonneuve P, Castellana P, Rotmensz N, Rossi S, Maggioni M, Persico M, Colombo A, Monasterolo F, Casadei-Giunchi D, et al. Incidence and risk factors for non-alcoholic steatohepatitis: prospective study of 5408 women enrolled in Italian tamoxifen chemoprevention trial. BMJ. 2005;330:932. [PMC free article] [PubMed] [Google Scholar]
11. Lonardo A, Trande P. Are there any sex differences in fatty liver? A study of glucose metabolism and body fat distribution. J Gastroenterol Hepatol. 2000;15:775–782. [PubMed] [Google Scholar]
12. Vernon G, Baranova A, Younossi ZM. Systematic review: the epidemiology and natural history of non-alcoholic fatty liver disease and non-alcoholic steatohepatitis in adults. Aliment Pharmacol Ther. 2011;34:274–285. [PubMed] [Google Scholar]
13. Turola E, Petta S, Vanni E, Milosa F, Valenti L, Critelli R, Miele L, Maccio L, Calvaruso V, Fracanzani AL, et al. Ovarian senescence increases liver fibrosis in humans and zebrafish with steatosis. Dis Model Mech. 2015;8:1037–1046. [PMC free article] [PubMed] [Google Scholar]
14. Klair JS, Yang JD, Abdelmalek MF, Guy CD, Gill RM, Yates K, Unalp-Arida A, Lavine JE, Clark JM, Diehl AM, et al. A longer duration of estrogen deficiency increases fibrosis risk among postmenopausal women with nonalcoholic fatty liver disease. Hepatology. 2016;64:85–91. [PMC free article] [PubMed] [Google Scholar]
15. Lonardo A, Bellentani S, Argo CK, Ballestri S, Byrne CD, Caldwell SH, Cortez-Pinto H, Grieco A, Machado MV, Miele L, et al. Epidemiological modifiers of non-alcoholic fatty liver disease: Focus on high-risk groups. Dig Liver Dis. 2015;47:997–1006. [PubMed] [Google Scholar]
16. Singh S, Allen AM, Wang Z, Prokop LJ, Murad MH, Loomba R. Fibrosis progression in nonalcoholic fatty liver vs nonalcoholic steatohepatitis: a systematic review and meta-analysis of paired-biopsy studies. Clin Gastroenterol Hepatol. 2015;13:643–654.e1-9; quiz e39-40. [PMC free article] [PubMed] [Google Scholar]
17. Dixon JB, Bhathal PS, O‘Brien PE. Nonalcoholic fatty liver disease: predictors of nonalcoholic steatohepatitis and liver fibrosis in the severely obese. Gastroenterology. 2001;121:91–100. [PubMed] [Google Scholar]
18. Wei JL, Leung JC, Loong TC, Wong GL, Yeung DK, Chan RS, Chan HL, Chim AM, Woo J, Chu WC, et al. Prevalence and Severity of Nonalcoholic Fatty Liver Disease in Non-Obese Patients: A Population Study Using Proton-Magnetic Resonance Spectroscopy. Am J Gastroenterol. 2015;110:1306–1314; quiz 1315. [PubMed] [Google Scholar]
19. Glass LM, Dickson RC, Anderson JC, Suriawinata AA, Putra J, Berk BS, Toor A. Total body weight loss of ≥ 10 % is associated with improved hepatic fibrosis in patients with nonalcoholic steatohepatitis. Dig Dis Sci. 2015;60:1024–1030. [PubMed] [Google Scholar]
20. Lonardo A, Sookoian S, Chonchol M, Loria P, Targher G. Cardiovascular and systemic risk in nonalcoholic fatty liver disease – atherosclerosis as a major player in the natural course of NAFLD. Curr Pharm Des. 2013;19:5177–5192. [PubMed] [Google Scholar]
21. Ballestri S, Nascimbeni F, Romagnoli D, Baldelli E, Lonardo A. The Role of Nuclear Receptors in the Pathophysiology, Natural Course, and Drug Treatment of NAFLD in Humans. Adv Ther. 2016;33:291–319. [PubMed] [Google Scholar]
22. Fazel Y, Koenig AB, Sayiner M, Goodman ZD, Younossi ZM. Epidemiology and natural history of non-alcoholic fatty liver disease. Metabolism. 2016;65:1017–1025. [PubMed] [Google Scholar]
23. Lonardo A, Bellentani S, Ratziu V, Loria P. Insulin resistance in nonalcoholic steatohepatitis: necessary but not sufficient – death of a dogma from analysis of therapeutic studies? Expert Rev Gastroenterol Hepatol. 2011;5:279–289. [PubMed] [Google Scholar]
24. Yilmaz Y. Review article: is non-alcoholic fatty liver disease a spectrum, or are steatosis and non-alcoholic steatohepatitis distinct conditions? Aliment Pharmacol Ther. 2012;36:815–823. [PubMed] [Google Scholar]
25. Pais R, Charlotte F, Fedchuk L, Bedossa P, Lebray P, Poynard T, Ratziu V. A systematic review of follow-up biopsies reveals disease progression in patients with non-alcoholic fatty liver. J Hepatol. 2013;59:550–556. [PubMed] [Google Scholar]
26. Wong VW, Wong GL, Choi PC, Chan AW, Li MK, Chan HY, Chim AM, Yu J, Sung JJ, Chan HL. Disease progression of non-alcoholic fatty liver disease: a prospective study with paired liver biopsies at 3 years. Gut. 2010;59:969–974. [PubMed] [Google Scholar]
27. McPherson S, Hardy T, Henderson E, Burt AD, Day CP, Anstee QM. Evidence of NAFLD progression from steatosis to fibrosing-steatohepatitis using paired biopsies: implications for prognosis and clinical management. J Hepatol. 2015;62:1148–1155. [PubMed] [Google Scholar]
28. Angulo P, Kleiner DE, Dam-Larsen S, Adams LA, Bjornsson ES, Charatcharoenwitthaya P, Mills PR, Keach JC, Lafferty HD, Stahler A, et al. Liver Fibrosis, but No Other Histologic Features, Is Associated With Long-term Outcomes of Patients With Nonalcoholic Fatty Liver Disease. Gastroenterology. 2015;149:389–397.e10. [PMC free article] [PubMed] [Google Scholar]
29. Ekstedt M, Hagström H, Nasr P, Fredrikson M, Stål P, Kechagias S, Hultcrantz R. Fibrosis stage is the strongest predictor for disease-specific mortality in NAFLD after up to 33 years of follow-up. Hepatology. 2015;61:1547–1554. [PubMed] [Google Scholar]
30. Lonardo A, Ballestri S, Marchesini G, Angulo P, Loria P. Nonalcoholic fatty liver disease: a precursor of the metabolic syndrome. Dig Liver Dis. 2015;47:181–190. [PubMed] [Google Scholar]
31. Oni ET, Agatston AS, Blaha MJ, Fialkow J, Cury R, Sposito A, Erbel R, Blankstein R, Feldman T, Al-Mallah MH, et al. A systematic review: burden and severity of subclinical cardiovascular disease among those with nonalcoholic fatty liver; should we care? Atherosclerosis. 2013;230:258–267. [PubMed] [Google Scholar]
32. Fargion S, Porzio M, Fracanzani AL. Nonalcoholic fatty liver disease and vascular disease: state-of-the-art. World J Gastroenterol. 2014;20:13306–13324. [PMC free article] [PubMed] [Google Scholar]
33. Loria P, Marchesini G, Nascimbeni F, Ballestri S, Maurantonio M, Carubbi F, Ratziu V, Lonardo A. Cardiovascular risk, lipidemic phenotype and steatosis. A comparative analysis of cirrhotic and non-cirrhotic liver disease due to varying etiology. Atherosclerosis. 2014;232:99–109. [PubMed] [Google Scholar]
34. Targher G, Day CP, Bonora E. Risk of cardiovascular disease in patients with nonalcoholic fatty liver disease. N Engl J Med. 2010;363:1341–1350. [PubMed] [Google Scholar]
35. Chen Y, Xu M, Wang T, Sun J, Sun W, Xu B, Huang X, Xu Y, Lu J, Li X, et al. Advanced fibrosis associates with atherosclerosis in subjects with nonalcoholic fatty liver disease. Atherosclerosis. 2015;241:145–150. [PubMed] [Google Scholar]
36. Sapmaz F, Uzman M, Basyigit S, Ozkan S, Yavuz B, Yeniova A, Kefeli A, Asilturk Z, Nazligül Y. Steatosis Grade is the Most Important Risk Factor for Development of Endothelial Dysfunction in NAFLD. Medicine (Baltimore) 2016;95:e3280. [PMC free article] [PubMed] [Google Scholar]
37. Lonardo A, Ballestri S, Targher G, Loria P. Diagnosis and management of cardiovascular risk in nonalcoholic fatty liver disease. Expert Rev Gastroenterol Hepatol. 2015;9:629–650. [PubMed] [Google Scholar]
38. Lonardo A, Sookoian S, Pirola CJ, Targher G. Non-alcoholic fatty liver disease and risk of cardiovascular disease. Metabolism. 2016;65:1136–1150. [PubMed] [Google Scholar]
39. Ballestri S, Lonardo A, Bonapace S, Byrne CD, Loria P, Targher G. Risk of cardiovascular, cardiac and arrhythmic complications in patients with non-alcoholic fatty liver disease. World J Gastroenterol. 2014;20:1724–1745. [PMC free article] [PubMed] [Google Scholar]
40. Valbusa F, Bonapace S, Grillo C, Scala L, Chiampan A, Rossi A, Zoppini G, Lonardo A, Arcaro G, Byrne CD, et al. Nonalcoholic Fatty Liver Disease Is Associated With Higher 1-year All-Cause Rehospitalization Rates in Patients Admitted for Acute Heart Failure. Medicine (Baltimore) 2016;95:e2760. [PMC free article] [PubMed] [Google Scholar]
41. Mantovani A, Rigamonti A, Bonapace S, Bolzan B, Pernigo M, Morani G, Franceschini L, Bergamini C, Bertolini L, Valbusa F, et al. Nonalcoholic Fatty Liver Disease Is Associated With Ventricular Arrhythmias in Patients With Type 2 Diabetes Referred for Clinically Indicated 24-Hour Holter Monitoring. Diabetes Care. 2016;39:1416–1423. [PubMed] [Google Scholar]
42. Giannini EG, Marabotto E, Savarino V, Trevisani F, di Nolfo MA, Del Poggio P, Benvegnù L, Farinati F, Zoli M, Borzio F, et al. Hepatocellular carcinoma in patients with cryptogenic cirrhosis. Clin Gastroenterol Hepatol. 2009;7:580–585. [PubMed] [Google Scholar]
43. Younossi ZM, Otgonsuren M, Henry L, Venkatesan C, Mishra A, Erario M, Hunt S. Association of nonalcoholic fatty liver disease (NAFLD) with hepatocellular carcinoma (HCC) in the United States from 2004 to 2009. Hepatology. 2015;62:1723–1730. [PubMed] [Google Scholar]
44. Piscaglia F, Svegliati-Baroni G, Barchetti A, Pecorelli A, Marinelli S, Tiribelli C, Bellentani S. Clinical patterns of hepatocellular carcinoma in nonalcoholic fatty liver disease: A multicenter prospective study. Hepatology. 2016;63:827–838. [PubMed] [Google Scholar]
45. Sangiovanni A, Colombo M. Surveillance for hepatocellular carcinoma: a standard of care, not a clinical option. Hepatology. 2011;54:1898–1900. [PubMed] [Google Scholar]
46. Michelini E, Lonardo A, Ballestri S, Costantini M, Caporali C, Bonati ME, Bertolotti M, Iori R, Loria P. Is cholangiocarcinoma another complication of insulin resistance: a report of three cases. Metab Syndr Relat Disord. 2007;5:194–202. [PubMed] [Google Scholar]
47. Welzel TM, Graubard BI, Zeuzem S, El-Serag HB, Davila JA, McGlynn KA. Metabolic syndrome increases the risk of primary liver cancer in the United States: a study in the SEER-Medicare database. Hepatology. 2011;54:463–471. [PMC free article] [PubMed] [Google Scholar]
48. Reddy SK, Hyder O, Marsh JW, Sotiropoulos GC, Paul A, Alexandrescu S, Marques H, Pulitano C, Barroso E, Aldrighetti L, et al. Prevalence of nonalcoholic steatohepatitis among patients with resectable intrahepatic cholangiocarcinoma. J Gastrointest Surg. 2013;17:748–755. [PMC free article] [PubMed] [Google Scholar]
49. Sanna C, Rosso C, Marietti M, Bugianesi E. Non-Alcoholic Fatty Liver Disease and Extra-Hepatic Cancers. Int J Mol Sci. 2016:17. [PMC free article] [PubMed] [Google Scholar]
50. Fukuda T, Hamaguchi M, Kojima T, Hashimoto Y, Ohbora A, Kato T, Nakamura N, Fukui M. The impact of non-alcoholic fatty liver disease on incident type 2 diabetes mellitus in non-overweight individuals. Liver Int. 2016;36:275–283. [PubMed] [Google Scholar]
51. Shah RV, Allison MA, Lima JA, Bluemke DA, Abbasi SA, Ouyang P, Jerosch-Herold M, Ding J, Budoff MJ, Murthy VL. Liver fat, statin use, and incident diabetes: The Multi-Ethnic Study of Atherosclerosis. Atherosclerosis. 2015;242:211–217. [PMC free article] [PubMed] [Google Scholar]
52. Sung KC, Wild SH, Byrne CD. Resolution of fatty liver and risk of incident diabetes. J Clin Endocrinol Metab. 2013;98:3637–3643. [PubMed] [Google Scholar]
53. Musso G, Gambino R, Cassader M, Pagano G. Meta-analysis: natural history of non-alcoholic fatty liver disease (NAFLD) and diagnostic accuracy of non-invasive tests for liver disease severity. Ann Med. 2011;43:617–649. [PubMed] [Google Scholar]
54. Yamazaki H, Tsuboya T, Tsuji K, Dohke M, Maguchi H. Independent Association Between Improvement of Nonalcoholic Fatty Liver Disease and Reduced Incidence of Type 2 Diabetes. Diabetes Care. 2015;38:1673–1679. [PubMed] [Google Scholar]
55. Hashimoto Y, Hamaguchi M, Fukuda T, Nakamura N, Ohbora A, Kojima T, Fukui M. BMI history and risk of incident fatty liver: a population-based large-scale cohort study. Eur J Gastroenterol Hepatol. 2016;28:1188–1193. [PubMed] [Google Scholar]
56. Ekstedt M, Franzén LE, Mathiesen UL, Thorelius L, Holmqvist M, Bodemar G, Kechagias S. Long-term follow-up of patients with NAFLD and elevated liver enzymes. Hepatology. 2006;44:865–873. [PubMed] [Google Scholar]
57. Leite NC, Villela-Nogueira CA, Cardoso CR, Salles GF. Non-alcoholic fatty liver disease and diabetes: from physiopathological interplay to diagnosis and treatment. World J Gastroenterol. 2014;20:8377–8392. [PMC free article] [PubMed] [Google Scholar]
58. Goh GB, Pagadala MR, Dasarathy J, Unalp-Arida A, Sargent R, Hawkins C, Sourianarayanane A, Khiyami A, Yerian L, Pai RK, et al. Clinical spectrum of non-alcoholic fatty liver disease in diabetic and non-diabetic patients. BBA Clin. 2015;3:141–145. [PMC free article] [PubMed] [Google Scholar]
59. Nascimbeni F, Aron-Wisnewsky J, Pais R, Tordjman J, Poitou C, Charlotte F, Bedossa P, Poynard T, Clément K, Ratziu V. Statins, antidiabetic medications and liver histology in patients with diabetes with non-alcoholic fatty liver disease. BMJ Open Gastroenterol. 2016;3:e000075. [PMC free article] [PubMed] [Google Scholar]
60. Ballestri S, Nascimbeni F, Romagnoli D, Baldelli E, Targher G, Lonardo A. Type 2 Diabetes in Non-Alcoholic Fatty Liver Disease and Hepatitis C Virus Infection–Liver: The “Musketeer” in the Spotlight. Int J Mol Sci. 2016;17:355. [PMC free article] [PubMed] [Google Scholar]
61. Oda K, Uto H, Mawatari S, Ido A. Clinical features of hepatocellular carcinoma associated with nonalcoholic fatty liver disease: a review of human studies. Clin J Gastroenterol. 2015;8:1–9. [PubMed] [Google Scholar]
62. Reeves HL, Zaki MY, Day CP. Hepatocellular Carcinoma in Obesity, Type 2 Diabetes, and NAFLD. Dig Dis Sci. 2016;61:1234–1245. [PubMed] [Google Scholar]
63. Zoppini G, Fedeli U, Gennaro N, Saugo M, Targher G, Bonora E. Mortality from chronic liver diseases in diabetes. Am J Gastroenterol. 2014;109:1020–1025. [PubMed] [Google Scholar]
64. Wild SH, Morling JR, McAllister DA, Kerssens J, Fischbacher C, Parkes J, Roderick PJ, Sattar N, Byrne CD. Type 2 diabetes and risk of hospital admission or death for chronic liver diseases. J Hepatol. 2016;64:1358–1364. [PubMed] [Google Scholar]
65. Ertle J, Dechêne A, Sowa JP, Penndorf V, Herzer K, Kaiser G, Schlaak JF, Gerken G, Syn WK, Canbay A. Non-alcoholic fatty liver disease progresses to hepatocellular carcinoma in the absence of apparent cirrhosis. Int J Cancer. 2011;128:2436–2443. [PubMed] [Google Scholar]
66. Sookoian S, Pirola CJ. Non-alcoholic fatty liver disease is strongly associated with carotid atherosclerosis: a systematic review. J Hepatol. 2008;49:600–607. [PubMed] [Google Scholar]
67. Mantovani A, Ballestri S, Lonardo A, Targher G. Cardiovascular Disease and Myocardial Abnormalities in Nonalcoholic Fatty Liver Disease. Dig Dis Sci. 2016;61:1246–1267. [PubMed] [Google Scholar]
68. Pais R, Giral P, Khan JF, Rosenbaum D, Housset C, Poynard T, Ratziu V. Fatty liver is an independent predictor of early carotid atherosclerosis. J Hepatol. 2016;65:95–102. [PubMed] [Google Scholar]
69. Ampuero J, Gallego-Durán R, Romero-Gómez M. Association of NAFLD with subclinical atherosclerosis and coronary-artery disease: meta-analysis. Rev Esp Enferm Dig. 2015;107:10–16. [PubMed] [Google Scholar]
70. Targher G, Bertolini L, Rodella S, Tessari R, Zenari L, Lippi G, Arcaro G. Nonalcoholic fatty liver disease is independently associated with an increased incidence of cardiovascular events in type 2 diabetic patients. Diabetes Care. 2007;30:2119–2121. [PubMed] [Google Scholar]
71. Jepsen P, Vilstrup H, Mellemkjaer L, Thulstrup AM, Olsen JH, Baron JA, Sørensen HT. Prognosis of patients with a diagnosis of fatty liver–a registry-based cohort study. Hepatogastroenterology. 2003;50:2101–2104. [PubMed] [Google Scholar]
72. Targher G, Bertolini L, Padovani R, Rodella S, Tessari R, Zenari L, Day C, Arcaro G. Prevalence of nonalcoholic fatty liver disease and its association with cardiovascular disease among type 2 diabetic patients. Diabetes Care. 2007;30:1212–1218. [PubMed] [Google Scholar]
73. Hamaguchi M, Kojima T, Takeda N, Nagata C, Takeda J, Sarui H, Kawahito Y, Yoshida N, Suetsugu A, Kato T, et al. Nonalcoholic fatty liver disease is a novel predictor of cardiovascular disease. World J Gastroenterol. 2007;13:1579–1584. [PMC free article] [PubMed] [Google Scholar]
74. Haring R, Wallaschofski H, Nauck M, Dörr M, Baumeister SE, Völzke H. Ultrasonographic hepatic steatosis increases prediction of mortality risk from elevated serum gamma-glutamyl transpeptidase levels. Hepatology. 2009;50:1403–1411. [PubMed] [Google Scholar]
75. Zhou YJ, Li YY, Nie YQ, Huang CM, Cao CY. Natural course of nonalcoholic fatty liver disease in southern China: a prospective cohort study. J Dig Dis. 2012;13:153–160. [PubMed] [Google Scholar]
76. Treeprasertsuk S, Leverage S, Adams LA, Lindor KD, St Sauver J, Angulo P. The Framingham risk score and heart disease in nonalcoholic fatty liver disease. Liver Int. 2012;32:945–950. [PMC free article] [PubMed] [Google Scholar]
77. Younossi ZM, Otgonsuren M, Venkatesan C, Mishra A. In patients with non-alcoholic fatty liver disease, metabolically abnormal individuals are at a higher risk for mortality while metabolically normal individuals are not. Metabolism. 2013;62:352–360. [PubMed] [Google Scholar]
78. Kim D, Kim WR, Kim HJ, Therneau TM. Association between noninvasive fibrosis markers and mortality among adults with nonalcoholic fatty liver disease in the United States. Hepatology. 2013;57:1357–1365. [PMC free article] [PubMed] [Google Scholar]
79. Pisto P, Santaniemi M, Bloigu R, Ukkola O, Kesäniemi YA. Fatty liver predicts the risk for cardiovascular events in middle-aged population: a population-based cohort study. BMJ Open. 2014;4:e004973. [PMC free article] [PubMed] [Google Scholar]
80. Pickhardt PJ, Hahn L, Muñoz del Rio A, Park SH, Reeder SB, Said A. Natural history of hepatic steatosis: observed outcomes for subsequent liver and cardiovascular complications. AJR Am J Roentgenol. 2014;202:752–758. [PubMed] [Google Scholar]
81. Moon SH, Hong SP, Cho YS, Noh TS, Choi JY, Kim BT, Lee KH. Hepatic FDG uptake is associated with future cardiovascular events in asymptomatic individuals with non-alcoholic fatty liver disease. J Nucl Cardiol. 2015 Epub ahead of print. [PubMed] [Google Scholar]
82. Fracanzani AL, Tiraboschi S, Pisano G, Consonni D, Baragetti A, Bertelli C, Norata D, Valenti L, Grigore L, Porzio M, et al. Progression of carotid vascular damage and cardiovascular events in non-alcoholic fatty liver disease patients compared to the general population during 10 years of follow-up. Atherosclerosis. 2016;246:208–213. [PubMed] [Google Scholar]
83. Dunn W, Xu R, Wingard DL, Rogers C, Angulo P, Younossi ZM, Schwimmer JB. Suspected nonalcoholic fatty liver disease and mortality risk in a population-based cohort study. Am J Gastroenterol. 2008;103:2263–2271. [PMC free article] [PubMed] [Google Scholar]
84. Wong VW, Wong GL, Yeung JC, Fung CY, Chan JK, Chang ZH, Kwan CT, Lam HW, Limquiaco J, Chim AM, et al. Long-term clinical outcomes after fatty liver screening in patients undergoing coronary angiogram: A prospective cohort study. Hepatology. 2016;63:754–763. [PubMed] [Google Scholar]
85. Adams LA, Lymp JF, St Sauver J, Sanderson SO, Lindor KD, Feldstein A, Angulo P. The natural history of nonalcoholic fatty liver disease: a population-based cohort study. Gastroenterology. 2005;129:113–121. [PubMed] [Google Scholar]
86. Rafiq N, Bai C, Fang Y, Srishord M, McCullough A, Gramlich T, Younossi ZM. Long-term follow-up of patients with nonalcoholic fatty liver. Clin Gastroenterol Hepatol. 2009;7:234–238. [PubMed] [Google Scholar]
87. Söderberg C, Stål P, Askling J, Glaumann H, Lindberg G, Marmur J, Hultcrantz R. Decreased survival of subjects with elevated liver function tests during a 28-year follow-up. Hepatology. 2010;51:595–602. [PubMed] [Google Scholar]
88. Targher G, Byrne CD, Lonardo A, Zoppini G, Barbui C. Non-alcoholic fatty liver disease and risk of incident cardiovascular disease: A meta-analysis. J Hepatol. 2016;65:589–600. [PubMed] [Google Scholar]
89. Sinn DH, Cho SJ, Gu S, Seong D, Kang D, Kim H, Yi BK, Paik SW, Guallar E, Cho J, et al. Persistent Nonalcoholic Fatty Liver Disease Increases Risk for Carotid Atherosclerosis. Gastroenterology. 2016;151:481–488.e1. [PubMed] [Google Scholar]
90. Bhatia L, Scorletti E, Curzen N, Clough GF, Calder PC, Byrne CD. Improvement in non-alcoholic fatty liver disease severity is associated with a reduction in carotid intima-media thickness progression. Atherosclerosis. 2016;246:13–20. [PubMed] [Google Scholar]
91. Samuel VT, Shulman GI. The pathogenesis of insulin resistance: integrating signaling pathways and substrate flux. J Clin Invest. 2016;126:12–22. [PMC free article] [PubMed] [Google Scholar]
92. Wang Y, Viscarra J, Kim SJ, Sul HS. Transcriptional regulation of hepatic lipogenesis. Nat Rev Mol Cell Biol. 2015;16:678–689. [PMC free article] [PubMed] [Google Scholar]
93. Lomonaco R, Bril F, Portillo-Sanchez P, Ortiz-Lopez C, Orsak B, Biernacki D, Lo M, Suman A, Weber MH, Cusi K. Metabolic Impact of Nonalcoholic Steatohepatitis in Obese Patients With Type 2 Diabetes. Diabetes Care. 2016;39:632–638. [PMC free article] [PubMed] [Google Scholar]
94. Meex RC, Hoy AJ, Morris A, Brown RD, Lo JC, Burke M, Goode RJ, Kingwell BA, Kraakman MJ, Febbraio MA, et al. Fetuin B Is a Secreted Hepatocyte Factor Linking Steatosis to Impaired Glucose Metabolism. Cell Metab. 2015;22:1078–1089. [PubMed] [Google Scholar]
95. Popov VB, Jornayvaz FR, Akgul EO, Kanda S, Jurczak MJ, Zhang D, Abudukadier A, Majumdar SK, Guigni B, Petersen KF, et al. Second-generation antisense oligonucleotides against β-catenin protect mice against diet-induced hepatic steatosis and hepatic and peripheral insulin resistance. FASEB J. 2016;30:1207–1217. [PMC free article] [PubMed] [Google Scholar]
96. Sepe PS, Ohri A, Sanaka S, Berzin TM, Sekhon S, Bennett G, Mehta G, Chuttani R, Kane R, Pleskow D, et al. A prospective evaluation of fatty pancreas by using EUS. Gastrointest Endosc. 2011;73:987–993. [PubMed] [Google Scholar]
97. Ou HY, Wang CY, Yang YC, Chen MF, Chang CJ. The association between nonalcoholic fatty pancreas disease and diabetes. PLoS One. 2013;8:e62561. [PMC free article] [PubMed] [Google Scholar]
98. Wu WC, Wang CY. Association between non-alcoholic fatty pancreatic disease (NAFPD) and the metabolic syndrome: case-control retrospective study. Cardiovasc Diabetol. 2013;12:77. [PMC free article] [PubMed] [Google Scholar]
99. Wang CY, Ou HY, Chen MF, Chang TC, Chang CJ. Enigmatic ectopic fat: prevalence of nonalcoholic fatty pancreas disease and its associated factors in a Chinese population. J Am Heart Assoc. 2014;3:e000297. [PMC free article] [PubMed] [Google Scholar]
100. Uygun A, Kadayifci A, Demirci H, Saglam M, Sakin YS, Ozturk K, Polat Z, Karslioglu Y, Bolu E. The effect of fatty pancreas on serum glucose parameters in patients with nonalcoholic steatohepatitis. Eur J Intern Med. 2015;26:37–41. [PubMed] [Google Scholar]
101. Yamazaki H, Tsuboya T, Katanuma A, Kodama Y, Tauchi S, Dohke M, Maguchi H. Lack of Independent Association Between Fatty Pancreas and Incidence of Type 2 Diabetes: 5-Year Japanese Cohort Study. Diabetes Care. 2016;39:1677–1683. [PubMed] [Google Scholar]
102. Pezzilli R, Calculli L. Pancreatic steatosis: Is it related to either obesity or diabetes mellitus? World J Diabetes. 2014;5:415–419. [PMC free article] [PubMed] [Google Scholar]
103. Back SH, Kaufman RJ. Endoplasmic reticulum stress and type 2 diabetes. Annu Rev Biochem. 2012;81:767–793. [PMC free article] [PubMed] [Google Scholar]
104. Loria P, Lonardo A, Anania F. Liver and diabetes. A vicious circle. Hepatol Res. 2013;43:51–64. [PMC free article] [PubMed] [Google Scholar]
105. Sharma RB, Alonso LC. Lipotoxicity in the pancreatic beta cell: not just survival and function, but proliferation as well? Curr Diab Rep. 2014;14:492. [PMC free article] [PubMed] [Google Scholar]
106. Sookoian S, Gianotti TF, Rosselli MS, Burgueño AL, Castaño GO, Pirola CJ. Liver transcriptional profile of atherosclerosis-related genes in human nonalcoholic fatty liver disease. Atherosclerosis. 2011;218:378–385. [PubMed] [Google Scholar]
107. Käräjämäki AJ, Bloigu R, Kauma H, Kesäniemi YA, Koivurova OP, Perkiömäki J, Huikuri H, Ukkola O. Non-alcoholic fatty liver disease with and without metabolic syndrome: Different long-term outcomes. Metabolism. 2016 [PubMed] [Google Scholar]
108. Lawlor DA, Callaway M, Macdonald-Wallis C, Anderson E, Fraser A, Howe LD, Day C, Sattar N. Nonalcoholic fatty liver disease, liver fibrosis, and cardiometabolic risk factors in adolescence: a cross-sectional study of 1874 general population adolescents. J Clin Endocrinol Metab. 2014;99:E410–E417. [PMC free article] [PubMed] [Google Scholar]
109. Adams LA. NAFLD. Accurate quantification of hepatic fat–is it important? Nat Rev Gastroenterol Hepatol. 2015;12:126–127. [PubMed] [Google Scholar]
110. Arulanandan A, Ang B, Bettencourt R, Hooker J, Behling C, Lin GY, Valasek MA, Ix JH, Schnabl B, Sirlin CB, et al. Association Between Quantity of Liver Fat and Cardiovascular Risk in Patients With Nonalcoholic Fatty Liver Disease Independent of Nonalcoholic Steatohepatitis. Clin Gastroenterol Hepatol. 2015;13:1513–1520.e1. [PubMed] [Google Scholar]
111. Soardo G, Donnini D, Domenis L, Catena C, De Silvestri D, Cappello D, Dibenedetto A, Carnelutti A, Bonasia V, Pagano C, et al. Oxidative stress is activated by free fatty acids in cultured human hepatocytes. Metab Syndr Relat Disord. 2011;9:397–401. [PubMed] [Google Scholar]
112. Leach NV, Dronca E, Vesa SC, Sampelean DP, Craciun EC, Lupsor M, Crisan D, Tarau R, Rusu R, Para I, et al. Serum homocysteine levels, oxidative stress and cardiovascular risk in non-alcoholic steatohepatitis. Eur J Intern Med. 2014;25:762–767. [PubMed] [Google Scholar]
113. Loomba R, Quehenberger O, Armando A, Dennis EA. Polyunsaturated fatty acid metabolites as novel lipidomic biomarkers for noninvasive diagnosis of nonalcoholic steatohepatitis. J Lipid Res. 2015;56:185–192. [PMC free article] [PubMed] [Google Scholar]
114. Luukkonen PK, Zhou Y, Sädevirta S, Leivonen M, Arola J, Orešič M, Hyötyläinen T, Yki-Järvinen H. Hepatic ceramides dissociate steatosis and insulin resistance in patients with non-alcoholic fatty liver disease. J Hepatol. 2016;64:1167–1175. [PubMed] [Google Scholar]
115. Gower E, Estes C, Blach S, Razavi-Shearer K, Razavi H. Global epidemiology and genotype distribution of the hepatitis C virus infection. J Hepatol. 2014;61:S45–S57. [PubMed] [Google Scholar]
116. Westbrook RH, Dusheiko G. Natural history of hepatitis C. J Hepatol. 2014;61:S58–S68. [PubMed] [Google Scholar]
117. Platt L, Easterbrook P, Gower E, McDonald B, Sabin K, McGowan C, Yanny I, Razavi H, Vickerman P. Prevalence and burden of HCV co-infection in people living with HIV: a global systematic review and meta-analysis. Lancet Infect Dis. 2016;16:797–808. [PubMed] [Google Scholar]
118. Aghemo A, Dore GJ, Hatzakis A, Wedemeyer H, Razavi H. Estimating HCV disease burden – volume 3 (editorial) J Viral Hepat. 2015;22 Suppl 4:1–3. [PubMed] [Google Scholar]
119. Bruno S, Di Marco V, Iavarone M, Roffi L, Crosignani A, Calvaruso V, Aghemo A, Cabibbo G, Viganò M, Boccaccio V, et al. Survival of patients with HCV cirrhosis and sustained virologic response is similar to the general population. J Hepatol. 2016;64:1217–1223. [PubMed] [Google Scholar]
120. Negro F, Forton D, Craxì A, Sulkowski MS, Feld JJ, Manns MP. Extrahepatic morbidity and mortality of chronic hepatitis C. Gastroenterology. 2015;149:1345–1360. [PubMed] [Google Scholar]
121. Lonardo A, Adinolfi LE, Petta S, Craxì A, Loria P. Hepatitis C and diabetes: the inevitable coincidence? Expert Rev Anti Infect Ther. 2009;7:293–308. [PubMed] [Google Scholar]
122. Younossi Z, Park H, Henry L, Adeyemi A, Stepanova M. Extrahepatic Manifestations of Hepatitis C: A Meta-analysis of Prevalence, Quality of Life, and Economic Burden. Gastroenterology. 2016;150:1599–1608. [PubMed] [Google Scholar]
123. Allison ME, Wreghitt T, Palmer CR, Alexander GJ. Evidence for a link between hepatitis C virus infection and diabetes mellitus in a cirrhotic population. J Hepatol. 1994;21:1135–1139. [PubMed] [Google Scholar]
124. Caronia S, Taylor K, Pagliaro L, Carr C, Palazzo U, Petrik J, O’Rahilly S, Shore S, Tom BD, Alexander GJ. Further evidence for an association between non-insulin-dependent diabetes mellitus and chronic hepatitis C virus infection. Hepatology. 1999;30:1059–1063. [PubMed] [Google Scholar]
125. Zein NN, Abdulkarim AS, Wiesner RH, Egan KS, Persing DH. Prevalence of diabetes mellitus in patients with end-stage liver cirrhosis due to hepatitis C, alcohol, or cholestatic disease. J Hepatol. 2000;32:209–217. [PubMed] [Google Scholar]
126. Knobler H, Stagnaro-Green A, Wallenstein S, Schwartz M, Roman SH. Higher incidence of diabetes in liver transplant recipients with hepatitis C. J Clin Gastroenterol. 1998;26:30–33. [PubMed] [Google Scholar]
127. Bigam DL, Pennington JJ, Carpentier A, Wanless IR, Hemming AW, Croxford R, Greig PD, Lilly LB, Heathcote JE, Levy GA, et al. Hepatitis C-related cirrhosis: a predictor of diabetes after liver transplantation. Hepatology. 2000;32:87–90. [PubMed] [Google Scholar]
128. Khalili M, Lim JW, Bass N, Ascher NL, Roberts JP, Terrault NA. New onset diabetes mellitus after liver transplantation: the critical role of hepatitis C infection. Liver Transpl. 2004;10:349–355. [PubMed] [Google Scholar]
129. Saliba F, Lakehal M, Pageaux GP, Roche B, Vanlemmens C, Duvoux C, Dumortier J, Salamé E, Calmus Y, Maugendre D. Risk factors for new-onset diabetes mellitus following liver transplantation and impact of hepatitis C infection : an observational multicenter study. Liver Transpl. 2007;13:136–144. [PubMed] [Google Scholar]
130. Knobler H, Schihmanter R, Zifroni A, Fenakel G, Schattner A. Increased risk of type 2 diabetes in noncirrhotic patients with chronic hepatitis C virus infection. Mayo Clin Proc. 2000;75:355–359. [PubMed] [Google Scholar]
131. Petit JM, Bour JB, Galland-Jos C, Minello A, Verges B, Guiguet M, Brun JM, Hillon P. Risk factors for diabetes mellitus and early insulin resistance in chronic hepatitis C. J Hepatol. 2001;35:279–283. [PubMed] [Google Scholar]
132. Hui JM, Sud A, Farrell GC, Bandara P, Byth K, Kench JG, McCaughan GW, George J. Insulin resistance is associated with chronic hepatitis C virus infection and fibrosis progression [corrected] Gastroenterology. 2003;125:1695–1704. [PubMed] [Google Scholar]
133. Lecube A, Hernández C, Genescà J, Esteban JI, Jardí R, Simó R. High prevalence of glucose abnormalities in patients with hepatitis C virus infection: a multivariate analysis considering the liver injury. Diabetes Care. 2004;27:1171–1175. [PubMed] [Google Scholar]
134. Moucari R, Asselah T, Cazals-Hatem D, Voitot H, Boyer N, Ripault MP, Sobesky R, Martinot-Peignoux M, Maylin S, Nicolas-Chanoine MH, et al. Insulin resistance in chronic hepatitis C: association with genotypes 1 and 4, serum HCV RNA level, and liver fibrosis. Gastroenterology. 2008;134:416–423. [PubMed] [Google Scholar]
135. Harrison SA. Correlation between insulin resistance and hepatitis C viral load. Hepatology. 2006;43:1168; author reply 1168–1169. [PubMed] [Google Scholar]
136. Hsu CS, Liu CJ, Liu CH, Wang CC, Chen CL, Lai MY, Chen PJ, Kao JH, Chen DS. High hepatitis C viral load is associated with insulin resistance in patients with chronic hepatitis C. Liver Int. 2008;28:271–277. [PubMed] [Google Scholar]
137. Mehta SH, Brancati FL, Sulkowski MS, Strathdee SA, Szklo M, Thomas DL. Prevalence of type 2 diabetes mellitus among persons with hepatitis C virus infection in the United States. Ann Intern Med. 2000;133:592–599. [PubMed] [Google Scholar]
138. Gray H, Wreghitt T, Stratton IM, Alexander GJ, Turner RC, O’Rahilly S. High prevalence of hepatitis C infection in Afro-Caribbean patients with type 2 diabetes and abnormal liver function tests. Diabet Med. 1995;12:244–249. [PubMed] [Google Scholar]
139. Simó R, Hernández C, Genescà J, Jardí R, Mesa J. High prevalence of hepatitis C virus infection in diabetic patients. Diabetes Care. 1996;19:998–1000. [PubMed] [Google Scholar]
140. Mason AL, Lau JY, Hoang N, Qian K, Alexander GJ, Xu L, Guo L, Jacob S, Regenstein FG, Zimmerman R, et al. Association of diabetes mellitus and chronic hepatitis C virus infection. Hepatology. 1999;29:328–333. [PubMed] [Google Scholar]
141. Mehta SH, Brancati FL, Strathdee SA, Pankow JS, Netski D, Coresh J, Szklo M, Thomas DL. Hepatitis C virus infection and incident type 2 diabetes. Hepatology. 2003;38:50–56. [PubMed] [Google Scholar]
142. Wang CS, Wang ST, Yao WJ, Chang TT, Chou P. Hepatitis C virus infection and the development of type 2 diabetes in a community-based longitudinal study. Am J Epidemiol. 2007;166:196–203. [PubMed] [Google Scholar]
143. White DL, Ratziu V, El-Serag HB. Hepatitis C infection and risk of diabetes: a systematic review and meta-analysis. J Hepatol. 2008;49:831–844. [PMC free article] [PubMed] [Google Scholar]
144. Fartoux L, Poujol-Robert A, Guéchot J, Wendum D, Poupon R, Serfaty L. Insulin resistance is a cause of steatosis and fibrosis progression in chronic hepatitis C. Gut. 2005;54:1003–1008. [PMC free article] [PubMed] [Google Scholar]
145. D’Souza R, Sabin CA, Foster GR. Insulin resistance plays a significant role in liver fibrosis in chronic hepatitis C and in the response to antiviral therapy. Am J Gastroenterol. 2005;100:1509–1515. [PubMed] [Google Scholar]
146. Muzzi A, Leandro G, Rubbia-Brandt L, James R, Keiser O, Malinverni R, Dufour JF, Helbling B, Hadengue A, Gonvers JJ, et al. Insulin resistance is associated with liver fibrosis in non-diabetic chronic hepatitis C patients. J Hepatol. 2005;42:41–46. [PubMed] [Google Scholar]
147. Petta S, Cammà C, Di Marco V, Alessi N, Cabibi D, Caldarella R, Licata A, Massenti F, Tarantino G, Marchesini G, et al. Insulin resistance and diabetes increase fibrosis in the liver of patients with genotype 1 HCV infection. Am J Gastroenterol. 2008;103:1136–1144. [PubMed] [Google Scholar]
148. Veldt BJ, Poterucha JJ, Watt KD, Wiesner RH, Hay JE, Rosen CB, Heimbach JK, Janssen HL, Charlton MR. Insulin resistance, serum adipokines and risk of fibrosis progression in patients transplanted for hepatitis C. Am J Transplant. 2009;9:1406–1413. [PubMed] [Google Scholar]
149. Veldt BJ, Chen W, Heathcote EJ, Wedemeyer H, Reichen J, Hofmann WP, de Knegt RJ, Zeuzem S, Manns MP, Hansen BE, et al. Increased risk of hepatocellular carcinoma among patients with hepatitis C cirrhosis and diabetes mellitus. Hepatology. 2008;47:1856–1862. [PubMed] [Google Scholar]
150. Chen CL, Yang HI, Yang WS, Liu CJ, Chen PJ, You SL, Wang LY, Sun CA, Lu SN, Chen DS, et al. Metabolic factors and risk of hepatocellular carcinoma by chronic hepatitis B/C infection: a follow-up study in Taiwan. Gastroenterology. 2008;135:111–121. [PubMed] [Google Scholar]
151. Hung CH, Wang JH, Hu TH, Chen CH, Chang KC, Yen YH, Kuo YH, Tsai MC, Lu SN, Lee CM. Insulin resistance is associated with hepatocellular carcinoma in chronic hepatitis C infection. World J Gastroenterol. 2010;16:2265–2271. [PMC free article] [PubMed] [Google Scholar]
152. Nkontchou G, Bastard JP, Ziol M, Aout M, Cosson E, Ganne-Carrie N, Grando-Lemaire V, Roulot D, Capeau J, Trinchet JC, et al. Insulin resistance, serum leptin, and adiponectin levels and outcomes of viral hepatitis C cirrhosis. J Hepatol. 2010;53:827–833. [PubMed] [Google Scholar]
153. Romero-Gómez M, Del Mar Viloria M, Andrade RJ, Salmerón J, Diago M, Fernández-Rodríguez CM, Corpas R, Cruz M, Grande L, Vázquez L, et al. Insulin resistance impairs sustained response rate to peginterferon plus ribavirin in chronic hepatitis C patients. Gastroenterology. 2005;128:636–641. [PubMed] [Google Scholar]
154. Poustchi H, Negro F, Hui J, Cua IH, Brandt LR, Kench JG, George J. Insulin resistance and response to therapy in patients infected with chronic hepatitis C virus genotypes 2 and 3. J Hepatol. 2008;48:28–34. [PubMed] [Google Scholar]
155. Dai CY, Huang JF, Hsieh MY, Hou NJ, Lin ZY, Chen SC, Hsieh MY, Wang LY, Chang WY, Chuang WL, et al. Insulin resistance predicts response to peginterferon-alpha/ribavirin combination therapy in chronic hepatitis C patients. J Hepatol. 2009;50:712–718. [PubMed] [Google Scholar]
156. Adinolfi LE, Zampino R, Restivo L, Lonardo A, Guerrera B, Marrone A, Nascimbeni F, Florio A, Loria P. Chronic hepatitis C virus infection and atherosclerosis: clinical impact and mechanisms. World J Gastroenterol. 2014;20:3410–3417. [PMC free article] [PubMed] [Google Scholar]
157. Petta S, Maida M, Macaluso FS, Barbara M, Licata A, Craxì A, Cammà C. Hepatitis C Virus Infection Is Associated With Increased Cardiovascular Mortality: A Meta-Analysis of Observational Studies. Gastroenterology. 2016;150:145–155.e4; quiz e15-16. [PubMed] [Google Scholar]
158. Kawaguchi T, Ide T, Taniguchi E, Hirano E, Itou M, Sumie S, Nagao Y, Yanagimoto C, Hanada S, Koga H, et al. Clearance of HCV improves insulin resistance, beta-cell function, and hepatic expression of insulin receptor substrate 1 and 2. Am J Gastroenterol. 2007;102:570–576. [PubMed] [Google Scholar]
159. Conjeevaram HS, Wahed AS, Afdhal N, Howell CD, Everhart JE, Hoofnagle JH. Changes in insulin sensitivity and body weight during and after peginterferon and ribavirin therapy for hepatitis C. Gastroenterology. 2011;140:469–477. [PubMed] [Google Scholar]
160. Arase Y, Suzuki F, Suzuki Y, Akuta N, Kobayashi M, Kawamura Y, Yatsuji H, Sezaki H, Hosaka T, Hirakawa M, et al. Sustained virological response reduces incidence of onset of type 2 diabetes in chronic hepatitis C. Hepatology. 2009;49:739–744. [PubMed] [Google Scholar]
161. Hsu YC, Lin JT, Ho HJ, Kao YH, Huang YT, Hsiao NW, Wu MS, Liu YY, Wu CY. Antiviral treatment for hepatitis C virus infection is associated with improved renal and cardiovascular outcomes in diabetic patients. Hepatology. 2014;59:1293–1302. [PubMed] [Google Scholar]
162. Hsu YC, Ho HJ, Huang YT, Wang HH, Wu MS, Lin JT, Wu CY. Association between antiviral treatment and extrahepatic outcomes in patients with hepatitis C virus infection. Gut. 2015;64:495–503. [PubMed] [Google Scholar]
163. Grasso A, Malfatti F, Testa R. Are metabolic factors still important in the era of direct antiviral agents in patients with chronic hepatitis C? World J Gastroenterol. 2013;19:6947–6956. [PMC free article] [PubMed] [Google Scholar]
164. Serfaty L, Forns X, Goeser T, Ferenci P, Nevens F, Carosi G, Drenth JP, Lonjon-Domanec I, DeMasi R, Picchio G, et al. Insulin resistance and response to telaprevir plus peginterferon α and ribavirin in treatment-naive patients infected with HCV genotype 1. Gut. 2012;61:1473–1480. [PubMed] [Google Scholar]
165. Pavone P, Tieghi T, d’Ettorre G, Lichtner M, Marocco R, Mezzaroma I, Passavanti G, Vittozzi P, Mastroianni CM, Vullo V. Rapid decline of fasting glucose in HCV diabetic patients treated with direct-acting antiviral agents. Clin Microbiol Infect. 2016;22:462.e1–462.e3. [PubMed] [Google Scholar]
166. Meissner EG, Lee YJ, Osinusi A, Sims Z, Qin J, Sturdevant D, McHutchison J, Subramanian M, Sampson M, Naggie S, et al. Effect of sofosbuvir and ribavirin treatment on peripheral and hepatic lipid metabolism in chronic hepatitis C virus, genotype 1-infected patients. Hepatology. 2015;61:790–801. [PMC free article] [PubMed] [Google Scholar]
167. Matsumori A, Yutani C, Ikeda Y, Kawai S, Sasayama S. Hepatitis C virus from the hearts of patients with myocarditis and cardiomyopathy. Lab Invest. 2000;80:1137–1142. [PubMed] [Google Scholar]
168. Boddi M, Abbate R, Chellini B, Giusti B, Solazzo V, Soft F, Pratesi G, Pratesi C, Gensini G, Zignego AL. HCV infection facilitates asymptomatic carotid atherosclerosis: preliminary report of HCV RNA localization in human carotid plaques. Dig Liver Dis. 2007;39 Suppl 1:S55–S60. [PubMed] [Google Scholar]
169. Sanchez MJ, Bergasa NV. Hepatitis C associated cardiomyopathy: potential pathogenic mechanisms and clinical implications. Med Sci Monit. 2008;14:RA55–RA63. [PubMed] [Google Scholar]
170. Boddi M, Abbate R, Chellini B, Giusti B, Giannini C, Pratesi G, Rossi L, Pratesi C, Gensini GF, Paperetti L, et al. Hepatitis C virus RNA localization in human carotid plaques. J Clin Virol. 2010;47:72–75. [PubMed] [Google Scholar]
171. Lonardo A, Adinolfi LE, Restivo L, Ballestri S, Romagnoli D, Baldelli E, Nascimbeni F, Loria P. Pathogenesis and significance of hepatitis C virus steatosis: an update on survival strategy of a successful pathogen. World J Gastroenterol. 2014;20:7089–7103. [PMC free article] [PubMed] [Google Scholar]
172. Maruyama S, Koda M, Oyake N, Sato H, Fujii Y, Horie Y, Murawaki Y. Myocardial injury in patients with chronic hepatitis C infection. J Hepatol. 2013;58:11–15. [PubMed] [Google Scholar]
173. Omran DA, Behairy NH, Zakaria KS, Nabil MM, Said K. Functional and morphological myocardial changes in hepatitis C virus patients with end-stage liver disease. Scand J Gastroenterol. 2015;50:1135–1143. [PubMed] [Google Scholar]
174. Tomiyama H, Arai T, Hirose K, Hori S, Yamamoto Y, Yamashina A. Hepatitis C virus seropositivity, but not hepatitis B virus carrier or seropositivity, associated with increased pulse wave velocity. Atherosclerosis. 2003;166:401–403. [PubMed] [Google Scholar]
175. Ishizaka N, Ishizaka Y, Takahashi E, Tooda Ei, Hashimoto H, Nagai R, Yamakado M. Association between hepatitis C virus seropositivity, carotid-artery plaque, and intima-media thickening. Lancet. 2002;359:133–135. [PubMed] [Google Scholar]
176. Targher G, Bertolini L, Padovani R, Rodella S, Arcaro G, Day C. Differences and similarities in early atherosclerosis between patients with non-alcoholic steatohepatitis and chronic hepatitis B and C. J Hepatol. 2007;46:1126–1132. [PubMed] [Google Scholar]
177. Mostafa A, Mohamed MK, Saeed M, Hasan A, Fontanet A, Godsland I, Coady E, Esmat G, El-Hoseiny M, Abdul-Hamid M, et al. Hepatitis C infection and clearance: impact on atherosclerosis and cardiometabolic risk factors. Gut. 2010;59:1135–1140. [PubMed] [Google Scholar]
178. Petta S, Torres D, Fazio G, Cammà C, Cabibi D, Di Marco V, Licata A, Marchesini G, Mazzola A, Parrinello G, et al. Carotid atherosclerosis and chronic hepatitis C: a prospective study of risk associations. Hepatology. 2012;55:1317–1323. [PubMed] [Google Scholar]
179. Adinolfi LE, Restivo L, Zampino R, Guerrera B, Lonardo A, Ruggiero L, Riello F, Loria P, Florio A. Chronic HCV infection is a risk of atherosclerosis. Role of HCV and HCV-related steatosis. Atherosclerosis. 2012;221:496–502. [PubMed] [Google Scholar]
180. Butt AA, Xiaoqiang W, Budoff M, Leaf D, Kuller LH, Justice AC. Hepatitis C virus infection and the risk of coronary disease. Clin Infect Dis. 2009;49:225–232. [PMC free article] [PubMed] [Google Scholar]
181. Lin MS, Guo SE, Chen MY, Huang TJ, Huang JC, Hu JH, Lin YS. The impact of hepatitis C infection on ischemic heart disease via ischemic electrocardiogram. Am J Med Sci. 2014;347:478–484. [PubMed] [Google Scholar]
182. Younossi ZM, Stepanova M, Nader F, Younossi Z, Elsheikh E. Associations of chronic hepatitis C with metabolic and cardiac outcomes. Aliment Pharmacol Ther. 2013;37:647–652. [PubMed] [Google Scholar]
183. Vassalle C, Masini S, Bianchi F, Zucchelli GC. Evidence for association between hepatitis C virus seropositivity and coronary artery disease. Heart. 2004;90:565–566. [PMC free article] [PubMed] [Google Scholar]
184. Alyan O, Kacmaz F, Ozdemir O, Deveci B, Astan R, Celebi AS, Ilkay E. Hepatitis C infection is associated with increased coronary artery atherosclerosis defined by modified Reardon severity score system. Circ J. 2008;72:1960–1965. [PubMed] [Google Scholar]
185. Satapathy SK, Kim YJ, Kataria A, Shifteh A, Bhansali R, Cerulli MA, Bernstein D. Higher Prevalence and More Severe Coronary Artery Disease in Hepatitis C Virus-infected Patients: A Case Control Study. J Clin Exp Hepatol. 2013;3:186–191. [PMC free article] [PubMed] [Google Scholar]
186. Pothineni NV, Delongchamp R, Vallurupalli S, Ding Z, Dai Y, Hagedorn CH, Mehta JL. Impact of hepatitis C seropositivity on the risk of coronary heart disease events. Am J Cardiol. 2014;114:1841–1845. [PMC free article] [PubMed] [Google Scholar]
187. McKibben RA, Haberlen SA, Post WS, Brown TT, Budoff M, Witt MD, Kingsley LA, Palella FJ, Thio CL, Seaberg EC. A Cross-sectional Study of the Association Between Chronic Hepatitis C Virus Infection and Subclinical Coronary Atherosclerosis Among Participants in the Multicenter AIDS Cohort Study. J Infect Dis. 2016;213:257–265. [PMC free article] [PubMed] [Google Scholar]
188. Yelken B, Gorgulu N, Caliskan Y, Elitok A, Cimen AO, Yazici H, Oflaz H, Turkmen A, Sever MS. Association between chronic hepatitis C infection and coronary flow reserve in dialysis patients with failed renal allografts. Transplant Proc. 2009;41:1519–1523. [PubMed] [Google Scholar]
189. Liao CC, Su TC, Sung FC, Chou WH, Chen TL. Does hepatitis C virus infection increase risk for stroke? A population-based cohort study. PLoS One. 2012;7:e31527. [PMC free article] [PubMed] [Google Scholar]
190. Adinolfi LE, Restivo L, Guerrera B, Sellitto A, Ciervo A, Iuliano N, Rinaldi L, Santoro A, Li Vigni G, Marrone A. Chronic HCV infection is a risk factor of ischemic stroke. Atherosclerosis. 2013;231:22–26. [PubMed] [Google Scholar]
191. Hsu CS, Kao JH, Chao YC, Lin HH, Fan YC, Huang CJ, Tsai PS. Interferon-based therapy reduces risk of stroke in chronic hepatitis C patients: a population-based cohort study in Taiwan. Aliment Pharmacol Ther. 2013;38:415–423. [PubMed] [Google Scholar]
192. Karibe H, Niizuma H, Ohyama H, Shirane R, Yoshimoto T. Hepatitis C virus (HCV) infection as a risk factor for spontaneous intracerebral hemorrhage: hospital based case-control study. J Clin Neurosci. 2001;8:423–425. [PubMed] [Google Scholar]
193. Tseng CH, Muo CH, Hsu CY, Kao CH. Increased Risk of Intracerebral Hemorrhage Among Patients With Hepatitis C Virus Infection. Medicine (Baltimore) 2015;94:e2132. [PMC free article] [PubMed] [Google Scholar]
194. Hsu YH, Muo CH, Liu CY, Tsai WC, Hsu CC, Sung FC, Kao CH. Hepatitis C virus infection increases the risk of developing peripheral arterial disease: a 9-year population-based cohort study. J Hepatol. 2015;62:519–525. [PubMed] [Google Scholar]
195. Guiltinan AM, Kaidarova Z, Custer B, Orland J, Strollo A, Cyrus S, Busch MP, Murphy EL. Increased all-cause, liver, and cardiac mortality among hepatitis C virus-seropositive blood donors. Am J Epidemiol. 2008;167:743–750. [PMC free article] [PubMed] [Google Scholar]
196. Lee MH, Yang HI, Wang CH, Jen CL, Yeh SH, Liu CJ, You SL, Chen WJ, Chen CJ. Hepatitis C virus infection and increased risk of cerebrovascular disease. Stroke. 2010;41:2894–2900. [PubMed] [Google Scholar]
197. Lee MH, Yang HI, Lu SN, Jen CL, You SL, Wang LY, Wang CH, Chen WJ, Chen CJ. Chronic hepatitis C virus infection increases mortality from hepatic and extrahepatic diseases: a community-based long-term prospective study. J Infect Dis. 2012;206:469–477. [PubMed] [Google Scholar]
198. Fernández-Montero JV, Barreiro P, de Mendoza C, Labarga P, Soriano V. Hepatitis C virus coinfection independently increases the risk of cardiovascular disease in HIV-positive patients. J Viral Hepat. 2016;23:47–52. [PubMed] [Google Scholar]
199. Fabrizi F, Dixit V, Messa P. Impact of hepatitis C on survival in dialysis patients: a link with cardiovascular mortality? J Viral Hepat. 2012;19:601–607. [PubMed] [Google Scholar]
200. Negro F. Facts and fictions of HCV and comorbidities: steatosis, diabetes mellitus, and cardiovascular diseases. J Hepatol. 2014;61:S69–S78. [PubMed] [Google Scholar]